United States to ban the TikTok too?
Biden signs a bill that could ban TikTok Washington: President Biden has signed into law a bill which gives the social media platform’s Chinese owner, ByteDance, nine months to divest the app or it will […]

Sam Pitroda stirs Indian election with wealth tax suggestion a la United States
‘Zindagi ke saath bhi, zindagi ke baad bhi’: PM Modi hits out at Congress New Delhi: Prime Minister Narendra Modi Thursday sharpened his attack on the Congress party as India goes to poll for […]

Universities taking measures against pro-Palestinian protests
– USC cancels graduation ceremony and dozens are arrested on other campuses – With graduation near, colleges seek to balance safety and students’ right to protest – Protests are carefully planned and improvised when needed […]

Indian restaurants in Colorado dupe investors of $3,80,000: Officials
New York: Two Indian restaurants in Colorado have duped investors to the tune of $3,80,000, state regulators have alleged and are now seeking to recover the amount from them. In a lawsuit, the Colorado Division […]

‘India may not travel to Pakistan for Champions Trophy’
New Delhi: Team India may not travel to Pakistan for the ICC Champions Trophy next year, and the venue for the event will likely get shifted or a hybrid model used, sources in the BCCI […]

IPL 2024: Rishabh Pant, Axar Patel help DC edge GT by 4 runs
New Delhi: Captain Rishabh Pant enthralled the home crowd by slamming an unbeaten 88 off 43 balls, while Axar Patel hit a 43-ball 66 and impact player Rasikh Salam picked a three-fer as Delhi Capitals […]
New York
Lahore Literary Festival 2024 to be held at Asia Society on April 27
New York: The Lahore Literary Festival (LLF), one of South Asia’s premier cultural events, is returning to Asia Society New York on April 27, exploring contemporary Pakistan through artists, writers, and other experts. The Lahore […]
NYC Health+Hospitals’ NYC Care program releases multilingual video series focused on membership card
NYC Health + Hospitals’ NYC Care program on April 10, 2024 announced the release of a video series focused on the NYC Care card and how to take advantage of one’s membership benefits. The videos […]
Mayor Adams releases Executive Budget for FY 2025
New York City Mayor Eric Adams released the City of New York’s balanced $111.6 B Fiscal Year (FY) 2025 Executive Budget. Mayor Adams’ budget builds on the administration’s actions, since last fall, to stabilize the […]
International
Pro-China Muizzu’s party sweeps Maldives elections
Male, Maldives: Maldives President Mohamed Muizzu’s political party has swept parliamentary elections in a strong endorsement of his pro-China foreign policy, according to preliminary results reported this week. The People’s National Congress won 70 out […]
About 1,300 people from Myanmar flee as clashes break out
Bangkok: About 1,300 people have fled from eastern Myanmar into Thailand, officials said, as fresh fighting erupted at a border town that was recently captured by ethnic rebels. Fighters from the Karen ethnic minority last […]
Imran Khan’s PTI denies secret talks with Pakistan’s powerful establishment
Islamabad: Jailed former prime minister Imran Khan-led Pakistan Tehreek-e-Insaf said that the party has no interest in engaging in discussions with anyone, firmly denying any rumors of secret negotiations with the powerful establishment. “Today, I […]
Pro-China Muizzu’s party sweeps Maldives elections
Male, Maldives: Maldives President Mohamed Muizzu’s political party has swept parliamentary elections in a strong endorsement of his pro-China foreign policy, according to preliminary results reported this week. The People’s National Congress won 70 out […]

About 1,300 people from Myanmar flee as clashes break out
Bangkok: About 1,300 people have fled from eastern Myanmar into Thailand, officials said, as fresh fighting erupted at a border town that was recently captured by ethnic rebels. Fighters from the Karen ethnic minority last […]
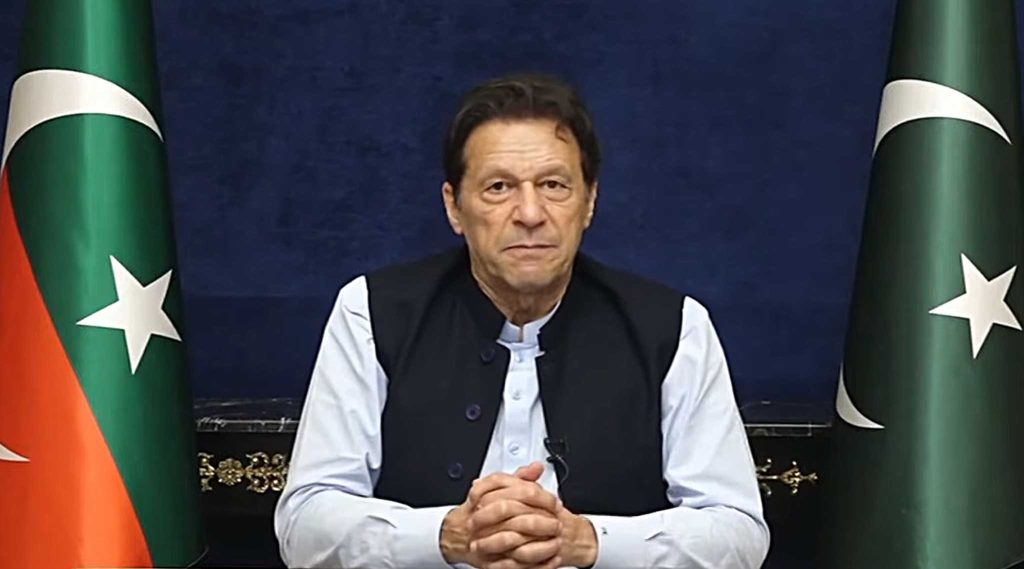
Imran Khan’s PTI denies secret talks with Pakistan’s powerful establishment
Islamabad: Jailed former prime minister Imran Khan-led Pakistan Tehreek-e-Insaf said that the party has no interest in engaging in discussions with anyone, firmly denying any rumors of secret negotiations with the powerful establishment. “Today, I […]

Pro-China Muizzu’s coalition wins Maldives elections
Male: Maldives President Mohamed Muizzu’s ruling coalition scored a landslide victory in April 21 parliamentary election, securing an absolute majority in Parliament as voters endorsed his government’s policy to align the Indian Ocean archipelago more […]

‘No power on earth can affect Iran-Pakistan ties’: President Raisi after US warning
New York: Iranian President Ebrahim Raisi, who has just concluded his three-day visit to Pakistan, asserted that “no power on Earth can affect the historical ties between the two countries”. His comment came hours after […]

Asia world’s most disaster-prone region in 2023: WMO
New York: Asia continued to bear the brunt of weather, climate, and water-related hazards in 2023, making it the world’s most disaster-hit region, according to a new report by the World Meteorological Organisation (WMO). Floods […]

Sam Pitroda stirs Indian election with wealth tax suggestion a la United States
‘Zindagi ke saath bhi, zindagi ke baad bhi’: PM Modi hits out at Congress New Delhi: Prime Minister Narendra Modi Thursday sharpened his attack on the Congress party as India goes to poll for […]
Pro-China Muizzu’s party sweeps Maldives elections
Male, Maldives: Maldives President Mohamed Muizzu’s political party has swept parliamentary elections in a strong endorsement of his pro-China foreign policy, according to preliminary results reported this week. The People’s National Congress won 70 out […]
India and the US are always stronger working together, says Eric Garcetti
New Delhi: Ambassador Eric Garcetti has said that climate action and green energy are some of the biggest pillars of the US-India alliance. In an interview to local media in India, the U.S. ambassador to […]

India 4th largest military spender in 2023: SIPRI
New Delhi: With military expenditure worth $83.6 billion in 2023, India was the fourth largest spender globally in 2023, the latest report by Stockholm International Peace Research Institute (SIPRI) states. This was a result of […]

CAA patently discriminatory, it must go: Chidambaram
New Delhi: Asserting that the Citizenship Amendment Act (CAA) is “patently discriminatory”, senior Congress leader P Chidambaram said his party’s position is that it must go and be replaced by a law of asylum which […]

Petition in SC demanding SIT probe into electoral bond scheme
New Delhi: The non-profit organization Common Cause and Centre for Public Interest Litigation (CPIL) have jointly moved a petition in the Supreme Court, demanding a probe by a special investigation team (SIT) under judicial supervision […]
Sam Pitroda stirs Indian election with wealth tax suggestion a la United States
‘Zindagi ke saath bhi, zindagi ke baad bhi’: PM Modi hits out at Congress New Delhi: Prime Minister Narendra Modi Thursday sharpened his attack on the Congress party as India goes to poll for […]
India and the US are always stronger working together, says Eric Garcetti
New Delhi: Ambassador Eric Garcetti has said that climate action and green energy are some of the biggest pillars of the US-India alliance. In an interview to local media in India, the U.S. ambassador to […]
India 4th largest military spender in 2023: SIPRI
New Delhi: With military expenditure worth $83.6 billion in 2023, India was the fourth largest spender globally in 2023, the latest report by Stockholm International Peace Research Institute (SIPRI) states. This was a result of […]
Entertainment
Parineeti Chopra weighs in on favoritism in Bollywood: ‘There are camps’
Parineeeti Chopra is currently receiving accolades for her performance in Imtiaz Ali’s ‘Amar Singh Chamkila’. Parineeti, who has seen several ups and downs in her career, has made some revelations about favoritism in Bollywood. The […]
‘12th Fail’ to release in over 20,000 screens in China, confirms Vikrant Massey
Vikrant Massey’s hit drama, ‘12th Fail’ is all set to release in China. The lead actors of the film, Vikrant and Medha Shankr are “excited and looking forward” to the same. In an exclusive interview […]
Ranbir, Ranveer, Yash, Allu Arjun in race for ‘Khalnayak 2’: Report
Filmmaker Subhash Ghai has finished the scripting of ‘Khalnayak 2’, the India Today reported citing a source. The director, who had made ‘Khalnayak’ with Sanjay Dutt over three decades ago, is also in talks with […]
Sports
‘India may not travel to Pakistan for Champions Trophy’
New Delhi: Team India may not travel to Pakistan for the ICC Champions Trophy next year, and the venue for the event will likely get shifted or a hybrid model used, sources in the BCCI […]
IPL 2024: Rishabh Pant, Axar Patel help DC edge GT by 4 runs
New Delhi: Captain Rishabh Pant enthralled the home crowd by slamming an unbeaten 88 off 43 balls, while Axar Patel hit a 43-ball 66 and impact player Rasikh Salam picked a three-fer as Delhi Capitals […]
IOC calls for Olympic Truce as Flame lit in Ancient Olympia for Paris 2024
Ancient Olympia (Greece): International Olympic Committee (IOC) president Thomas Bach and other IOC high officials called for world peace on Tuesday during the flame-lighting ceremony for the 2024 Paris Olympics in Ancient Olympia, Greece. The […]
Business
US economic growth in first quarter falls short of expectations
New York: The US economy expanded less than projected in the first three months of 2024 as exports and consumer spending declined, according to the Commerce Department. The first quarter saw the world’s largest economy […]
RBI bars Kotak Mahindra Bank from onboarding new customers online
Mumbai: The Reserve Bank of India (RBI) has directed Kotak Mahindra Bank Limited to stop onboarding of new customers through its online and mobile banking with immediate effect and also barred the bank from issuing […]
IMF increases India’s growth projection to 6.8% for 2024
Washington: The International Monetary Fund (IMF) has pegged India’s growth projection to 6.8 pc this year, an increase of 0.3 pc over its January 2024 update. The IMF in its World Economic Outlook (WEO) said […]
Lifestyle
Time spent in natural surroundings lowers heart disease, diabetes risk
Do you enjoy your time spent in nature? It may help lower inflammation levels, linked to the risk of heart disease and diabetes, finds a study. While previous research linked exposure to the natural world […]
India’s Rasmalai takes second spot in world’s ‘Top 10 best cheese desserts’
Beyond the classic flavors and textures of chocolate and blueberries, cheese desserts are available in a multitude of combinations. The variety of cheese in culinary pleasures is exhibited by these goodies, which range from rich […]
From Riches to Renunciation: Gujarat Couple Donates Rs 200 cr to Embrace Monkhood
A Jain couple from Gujarat has captured headlines for their extraordinary decision to renounce their material wealth and pursue a life of spiritual devotion. Bhavesh Bhandari, a successful businessman from Himmatnagar, and his wife recently […]